There have been various attempts to measure productivity in the NHS since the 1980s using different approaches to aggregate NHS activity (outputs) and divide it by NHS inputs (physical inputs, mainly staff). Whichever method is used, the historic trend is relatively modest – on average productivity has grown by around 1 per cent each year.
However, look a little closer and there are parts of the health service that have seen remarkable improvements in performance.
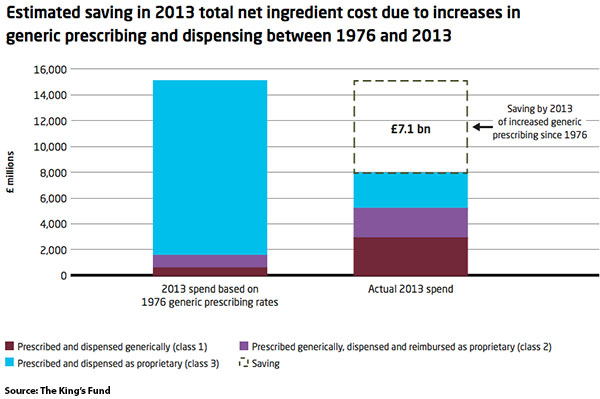
Take prescribing as an example. The proportion of drugs prescribed in their generic form, rather than their chemically identical (but more expensive) branded alternative, increased from 20 to 83 per cent between 1976 and 2013, providing significantly more value from the NHS prescribing budget. If we look at what the prescribing spend in 2013 would have been if generic prescribing levels had stayed at their 1976 rate (see figure below), we find that the NHS effectively saved £7.1 billion because of the change in prescribing practice. Put another way, almost half a million more items were prescribed for the same budget because of the switch to generics.
Significant growth has also been seen in the proportion of patients who are admitted, treated and discharged from hospital on the same day. While 7 per cent of all patient activity was carried out as day cases in 1974, by 2013/14 that figure had risen to 35 per cent. And for some procedures, almost all activity is now completed within a day – 98 per cent of all elective cataract operations, for example, are now conducted as day cases.
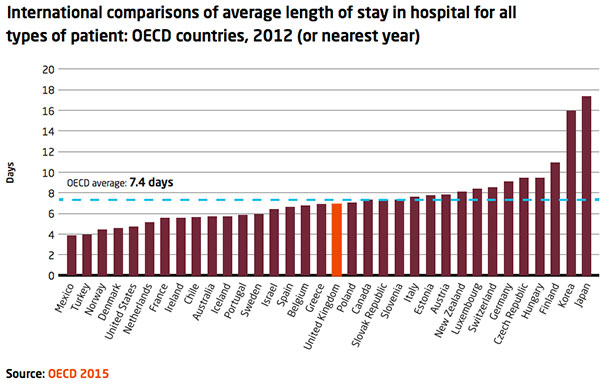
In a similar vein, the average length of stay in hospital for medical and surgical in-patients has decreased from 10.4 days in 1974, to just 4 days in 2013. These improvements are even more impressive given that, over the same period, the in-patient case mix has become more complex, with simpler cases now more often treated as day cases.
In all of these areas, there is still potential for further improvement. The chart below shows that the UK sits around the middle of the international league table on length of stay. If the health service in England managed, for example, to reduce length of stay by a further 15 per cent by 2023, it would be able to treat 18 per cent more patients within the same overall budget.
How can these stories from the past help the NHS as it seeks to meet the challenge set out in Simon Steven’s plan for the NHS’ future, to deliver £22bn in productivity savings by 2020? The first lesson from these past successes is that the drivers of change are multiple; they include technical, cultural, political, financial and policy factors and they are often overlapping. Improvements in pain relief medications and in surgical techniques, for example, were key to the shift in activity from in-patient to day cases. However that shift would not have happened without close collaboration between managers and clinicians to implement changes to the way care is provided. Among other factors, the payment by results tariff – which determines how much hospitals are paid for carrying out treatments – also played an important role. In 2005/06 a tariff was rolled out for all elective procedures that reimbursed hospitals for day cases at a rate based on the average of the in-patient and day-case cost combined. This created an in-built financial incentive for hospitals to switch to day-case work.
The King’s Fund report, Better value in the NHS, is available to download




















